Healthcare organizations are heading toward a perfect storm. Denials are rising, payer policies are shifting faster than providers can keep up, workforce shortages are straining accuracy, and major CPT code changes will hit in 2026, putting massive pressure on revenue cycle management (RCM) teams.
The result? Revenue leakage is accelerating, costing hospitals and medical groups millions every year. Research shows that healthcare organizations lose 5–10% of net revenue to inefficiencies, denials, underpayments, and operational blind spots that are often entirely preventable.
If your organization wants to stay financially strong heading into 2026, sealing revenue leaks isn’t optional, it’s urgent.
This in-depth guide breaks down the 12 most costly RCM revenue leaks, explains why each is getting worse, and provides actionable solutions you can implement now to protect your bottom line before 2026.
1. Rising Payer Denials (Medical Necessity, Clinical Validation, Bundling)
Payer denials remain the single largest source of financial waste in healthcare.
Why it’s Getting Worse
- Payers are tightening medical necessity rules.
- Clinical validation demands are rising.
- Bundling and coding logic changes are becoming more aggressive.
- AI-driven denials are increasing volume and speed.
How to Fix This
- Deploy real-time denial analytics.
- Build prebill clinical validation workflows.
- Automate payer policy updates.
- Negotiate contract clauses to limit denial rates.
- Strengthen documentation templates.
Recommended Reading:
For organizations exploring outsourced support for denial management, review how outsourcing strengthens operational efficiency:
👉 How Outsourcing RCM Improves Financial Health
2. Authorization Failures & Eligibility Errors
Among the costliest front-end leaks, unauthorized services often result in zero reimbursement.
Why it’s Getting Worse
- Shortened authorization windows.
- More frequent reauthorizations.
- High staff turnover.
- Outpatient shift increases auth requirements.
How to Fix This
- Automate eligibility at scheduling, preregistration, and DOS.
- Centralize authorization departments.
- Use AI to detect missing authorizations.
- Standardize workflows by CPT code.
3. Inaccurate or Missed Charge Capture
Charge capture errors can cost organizations millions annually.
Why it’s Getting Worse
- 2026 CPT changes increase complexity.
- More outpatient services → more manual charging errors.
- Surgery and infusion remain highly error-prone.
How to Fix This
- Automate charge reconciliation.
- Audit high-risk departments monthly.
- Use charge lag dashboards.
- Train clinicians on documentation tied to charging accuracy.
4. Underpayments & Payer Contract Noncompliance
One of the most silent revenue leaks, claims appear paid but are under-reimbursed.
Why it’s Getting Worse
- Automated payer adjudication changes.
- Outdated contract modeling.
- Growing outpatient complexity.
How to Fix This
- Use contract analytics software.
- Conduct quarterly underpayment sweeps.
- Add reimbursement variance alerts.
- Strengthen payer negotiations.
5. Coding Errors & Documentation Gaps
Coding accuracy impacts DRGs, HCCs, risk adjustment, and reimbursement.
Why it’s Getting Worse
- Coding updates in 2026.
- Increased payer scrutiny.
- Staffing shortages.
- Documentation inconsistencies.
How to Fix This
- Expand CDI into outpatient.
- Use AI-assisted coding review tools.
- Provide specialty-based documentation templates.
6. Failures in Point-of-Service Collections
With patient responsibility rising, POS failures cause irrecoverable losses.
Why it’s Getting Worse
- Higher deductibles.
- Poor accuracy of cost estimates.
- Lack of financial counseling training.
How to Fix This
- Use real-time cost estimators.
- Train staff in payment expectation scripts.
- Offer digital billing + payment plans.
7. Data Quality Errors in Patient Demographics
Small demographic errors lead to costly rejections and denials.
Why it’s Getting Worse
- Registration turnover.
- Multi-system data mismatches.
- Tighter payer matching algorithms.
How to Fix This
- Automate demographic verification.
- Standardize registration fields.
- Hold quarterly demographic audits.
8. Lack of Real-Time RCM Visibility
Many teams rely on lagging indicators, causing delayed responses.
Why it’s Getting Worse
- Manual reporting delays.
- Siloed systems.
- Higher outpatient volumes.
How to Fix This
- Use real-time dashboards.
- Apply denial forecasting.
- Review KPIs weekly.
- Create payer scorecards.
9. Slow or Ineffective AR Follow-Up
Delayed AR follow-up directly reduces cash flow.
Why it’s Getting Worse
- Staff shortages.
- Shorter appeal windows.
- Auto-closed claims from payers.
How to Fix This
- Automate claim-status checks.
- Segment AR into high vs. low-yield.
- Standardize escalation workflows.
10. Missed Preventive & Chronic Care Billing Opportunities
A major leak in ambulatory environments.
Why it’s Getting Worse
- Underutilization of CCM/RPM codes.
- Documentation complexity.
- Lack of provider awareness.
How to Fix This
- Automate eligibility detection.
- Track gaps via dashboards.
- Educate providers on billing rules.
11. Payer Noncompliance with CMS Regulations
Payers often misapply CMS rules, which forces providers to absorb costs.
Why it’s Getting Worse
- NSA and transparency rule confusion.
- Payer misinterpretation driving denials.
- Limited internal payer auditing.
How to Fix This
- Conduct payer compliance audits.
- Identify patterns of inappropriate denials.
- Enforce stronger contract protections.
12. Inefficient Manual Workflows Across RCM
Manual processes cannot keep pace with automated payers.
Why it’s Getting Worse
- Workforce shortages.
- Higher volumes.
- Increased payer automation.
How to Fix This
- Map and automate manual workflows.
- Use AI for coding review, routing, and documentation requests.
- Deploy RPA for payment posting and status checks.
How to Prioritize Fixing Revenue Leaks Before 2026
To effectively address revenue leakage:
✔ Conduct a full leakage audit
(front-end → mid-cycle → back-end)
✔ Build a high-impact priority matrix
Focus on high-dollar + high-frequency leaks.
✔ Modernize systems before CPT 2026 changes
Your tech stack must be ready beforehand.
✔ Strengthen cross-functional alignment
Revenue protection is not just an RCM issue; it’s an organizational one.
What You Can Do Right Now
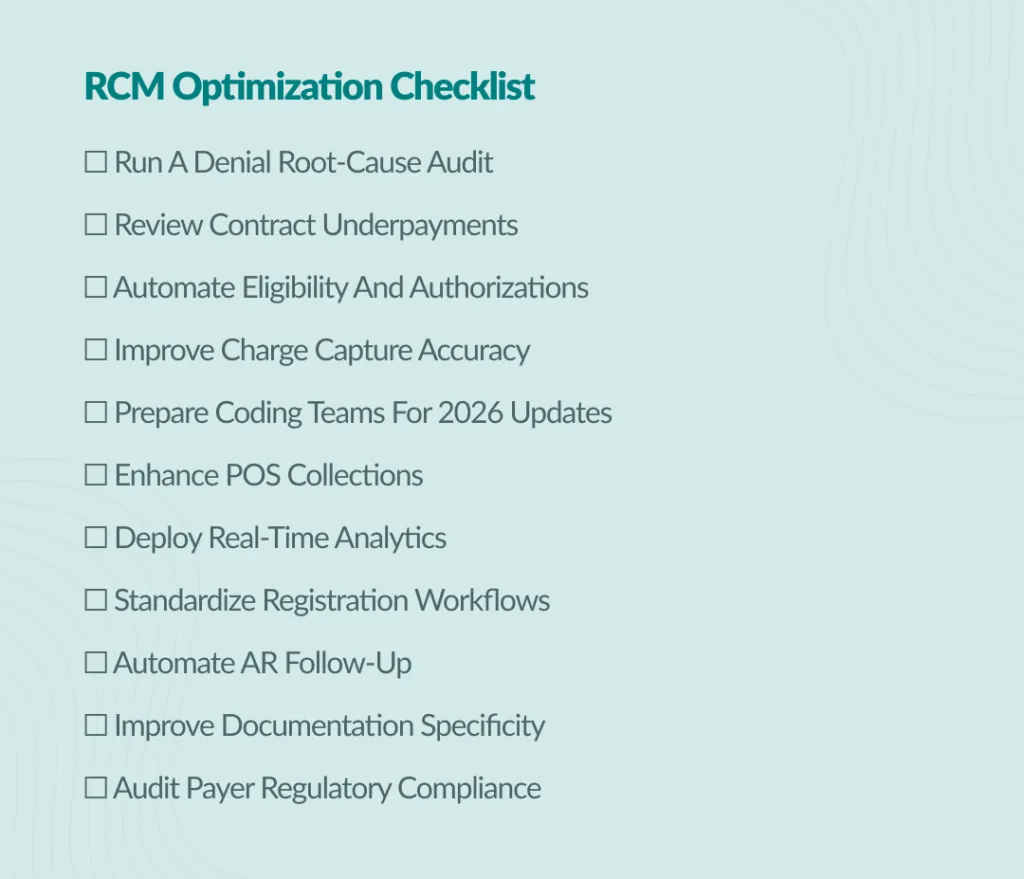
Here’s a checklist for RCM optimization:
Stronger Revenue Cycle Performance Starts with a Strong Partner
If your organization needs support preparing for 2026, managing denials, improving clinical documentation, or reducing revenue leakage, Medviz Systems provides comprehensive solutions designed to strengthen financial health.
Explore our complete offering:
👉 Medviz Revenue Cycle Management Services
And if you’d like to see how outsourcing strengthens both financial and patient-facing outcomes, read:
👉 How Outsourcing RCM Improves Patient Satisfaction and Financial Health
Ready to Seal Your Revenue Leaks Before 2026?
Medviz Systems empowers healthcare organizations to:
✔ Reduce denials
✔ Improve cash flow
✔ Boost coding accuracy
✔ Enhance front-end & back-end efficiency
✔ Prepare for CPT 2026 changes
✔ Strengthen the entire revenue cycle
Contact Medviz today to schedule your Revenue Leakage Assessment.
Call +1 (727) 214-2749 or email success@medviz.ai to learn how Medviz Systems can streamline your coding workflows, minimize denials, and help your practice stay audit-ready while maximizing profitability.
Leave a Reply to The Ultimate 2026 Audit-Proofing Guide for Clinics | Compliance & RCM Cancel reply