Clinical notes are a foundational element of healthcare documentation, playing a critical role in ensuring safe, effective, and compliant patient care. Whether you’re a physician, nurse, therapist, medical student, or healthcare administrator, mastering clinical notetaking is essential to delivering high-quality care. But what exactly is a clinical note, and why is it so crucial?
In this article, we’ll define clinical notes, explore their significant role in healthcare, and break down the most common types. We’ll also highlight how AI-powered clinical documentation is transforming the industry. By the end, you’ll have a comprehensive understanding of how clinical notes support patient care, ensure regulatory compliance, assist clinical decision-making, and help reduce the administrative burden on healthcare providers.
What Is a Clinical Note?
A clinical note is a formal written or electronic record created by a healthcare professional to document a patient’s condition, assessment, treatment, and ongoing progress. Clinical notes are a core component of the patient’s medical record and are typically maintained within an electronic health record (EHR) or electronic medical record (EMR) system.
Clinical notes may be written by a wide range of licensed healthcare providers, including:
- Physicians
- Nurses
- Mental health professionals
- Physical, occupational, and speech therapists
- Nurse practitioners and physician assistants
Unlike informal or personal notes, clinical notes follow strict professional, legal, and regulatory standards. They serve multiple critical purposes, including communicating patient information across care teams, guiding clinical decision-making, supporting billing and reimbursement, and providing legally defensible documentation.
What Is the Purpose of a Clinical Note?
The purpose of a clinical note extends far beyond basic recordkeeping. Accurate and timely clinical documentation plays a critical role in patient safety, quality of care, and overall organizational efficiency.
Key purposes of clinical notes include:
- Continuity of care
Clinical notes ensure that all healthcare providers involved in a patient’s care have access to consistent, up-to-date information, supporting coordinated treatment across settings. - Clinical decision-making
Well-documented assessments and care plans help clinicians make accurate diagnoses and informed treatment decisions. - Legal and regulatory protection
Clinical notes are legal documents that may be reviewed during audits, regulatory investigations, or malpractice claims, making accuracy and completeness essential. - Billing and reimbursement
Insurance payers rely on clinical notes to verify medical necessity and justify reimbursement for services provided. - Quality improvement and research
Aggregated clinical documentation data supports outcome tracking, performance measurement, and system-wide quality improvement initiatives.
Clear, well-structured documentation protects both patients and healthcare professionals while strengthening the overall delivery of care.
What Should Be Included in a Clinical Note?
While clinical note formats vary by specialty and care setting, most clinical notes share essential components that support clarity, accuracy, and regulatory compliance.
Standard elements of a clinical note include:
- Patient identifiers
Name, date of birth, and medical record number. - Date, time, and author credentials
When the note was created and the credentials of the documenting provider. - Subjective information
Patient-reported symptoms, concerns, or relevant history. - Objective findings
Physical examination results, vital signs, laboratory data, and other measurable observations. - Assessment
Diagnoses, clinical impressions, or identified problems. - Plan of care
Treatments, medications, referrals, patient education, and follow-up plans. - Authentication
Provider signature or electronic verification to confirm accuracy and accountability.
Including these elements helps ensure clinical notes meet professional standards, support effective communication, and comply with regulatory requirements.
Types of Clinical Notes Used in Healthcare
Healthcare professionals use a variety of clinical note types depending on the care setting, specialty, and purpose of documentation. Each type of clinical note serves a distinct role in supporting patient care, clinical decision-making, compliance, and communication across healthcare teams.
History and Physical (H&P) Note
The History and Physical (H&P) note is a comprehensive, foundational clinical document typically completed at the time of hospital admission, prior to surgery, or at the start of a new episode of care. Its primary purpose is to establish a detailed clinical baseline for the patient.
Key components of an H&P note include:
- Chief complaint and reason for encounter
- History of present illness (HPI)
- Past medical, surgical, family, and social history
- Review of systems (ROS)
- Physical examination findings
- Initial assessment and differential diagnoses
- Preliminary treatment and care plan
H&P notes are critical for care planning, risk assessment, and regulatory compliance, particularly in inpatient and surgical settings.
SOAP Notes
SOAP notes are one of the most widely used clinical note formats across outpatient, inpatient, and specialty care settings. The SOAP structure provides a standardized approach to documenting patient encounters.
SOAP stands for:
- Subjective: Patient-reported symptoms, concerns, and history
- Objective: Measurable findings such as vitals, exam results, and labs
- Assessment: Clinical interpretation, diagnoses, or problem list
- Plan: Treatments, medications, referrals, and follow-up care
SOAP notes are especially effective for tracking patient progress over time and supporting clear, organized clinical reasoning.
Progress Notes
Progress notes document a patient’s clinical status throughout the course of care. They are typically written daily in inpatient settings or at each visit in outpatient care.
Progress notes may include:
- Changes in symptoms or condition
- Patient response to treatments or medications
- Updated assessments or diagnoses
- Modifications to the treatment plan
These notes support continuity of care and help providers evaluate whether current interventions are effective.
Discharge Notes
Discharge notes are completed at the conclusion of a patient encounter or hospital stay. They provide a comprehensive summary of the care provided and ensure continuity as the patient transitions to the next level of care.
Discharge notes typically document:
- Reason for admission or visit
- Final diagnoses
- Procedures or treatments performed
- Medications at discharge
- Follow-up instructions and referrals
- Patient education provided
Clear discharge notes are essential for patient safety, reducing readmissions, and ensuring proper follow-up care.
Specialty-Specific Clinical Notes
Many healthcare disciplines use specialized clinical note formats tailored to their unique documentation needs and regulatory requirements.
Common specialty-specific notes include:
- DAP and BIRP notes in mental and behavioral health, focusing on interventions and patient response
- Nursing notes, which document patient status, care provided, and response to interventions
- Therapy notes used in physical, occupational, and speech therapy to track functional progress and treatment outcomes
These specialized notes enhance interdisciplinary communication and ensure documentation aligns with professional standards.
Why Understanding Clinical Note Types Matters
Understanding the different types of clinical notes helps healthcare professionals deliver safer, more efficient, and higher-quality care. Clear knowledge of clinical documentation enables providers to:
- Communicate more effectively across care teams, ensuring continuity and coordination of care
- Maintain regulatory and legal compliance with documentation standards
- Improve documentation accuracy and efficiency, reducing errors and rework
- Support better patient outcomes through informed clinical decision-making
Well-structured clinical documentation is a cornerstone of high-quality healthcare delivery and plays a critical role in patient safety and organizational performance.
The Documentation Burden: A Growing Crisis
Physician burnout is accelerating as administrative demands continue to rise. Clinicians now spend nearly two hours on EHR documentation for every one hour of direct patient care, which significantly reduces the time available for meaningful patient interactions. In fact, 44% of a physician’s workday is devoted to paperwork rather than patient care, making documentation burden one of the leading causes of physician burnout.
This growing imbalance has created an urgent demand for technological solutions that reduce documentation time while maintaining or improving the quality and accuracy of clinical notes.
AI-Powered Clinical Documentation: A Solution to the Burden
Artificial Intelligence is revolutionizing clinical documentation by automating the most time-consuming aspects of medical note creation. AI clinical documentation tools reduce administrative burden, improve note quality, and allow clinicians to spend more time focused on patient care.
Modern solutions rely on a combination of advanced technologies that work together to capture, interpret, and generate accurate clinical notes in real time.
Core Technologies Behind AI Clinical Documentation
End-to-End Documentation Workflow
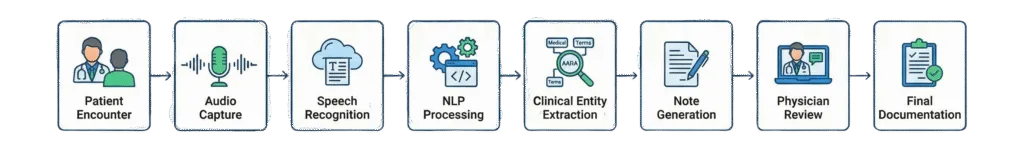
This streamlined workflow ensures clinical accuracy while minimizing manual effort.
1. Automatic Speech Recognition (ASR)
Automatic Speech Recognition converts spoken conversations between patients and providers into text with medical-grade accuracy. These systems recognize complex medical terminology, drug names, acronyms, and anatomical references, even in fast-paced clinical environments.
2. Natural Language Processing (NLP)
Natural Language Processing analyzes the transcribed conversation to extract meaningful clinical data, including:
- Clinical entities such as symptoms, diagnoses, medications, and allergies
- Temporal references such as “started three days ago”
- Severity, duration, and modifying factors
- Distinction between patient-reported information and clinician observations
This step ensures that unstructured dialogue becomes structured clinical data.
3. Large Language Models (LLMs)
Large Language Models transform extracted clinical data into coherent, well-structured medical notes. These notes follow established formats such as SOAP, H&P, or progress notes and adapt to specialty-specific documentation standards.
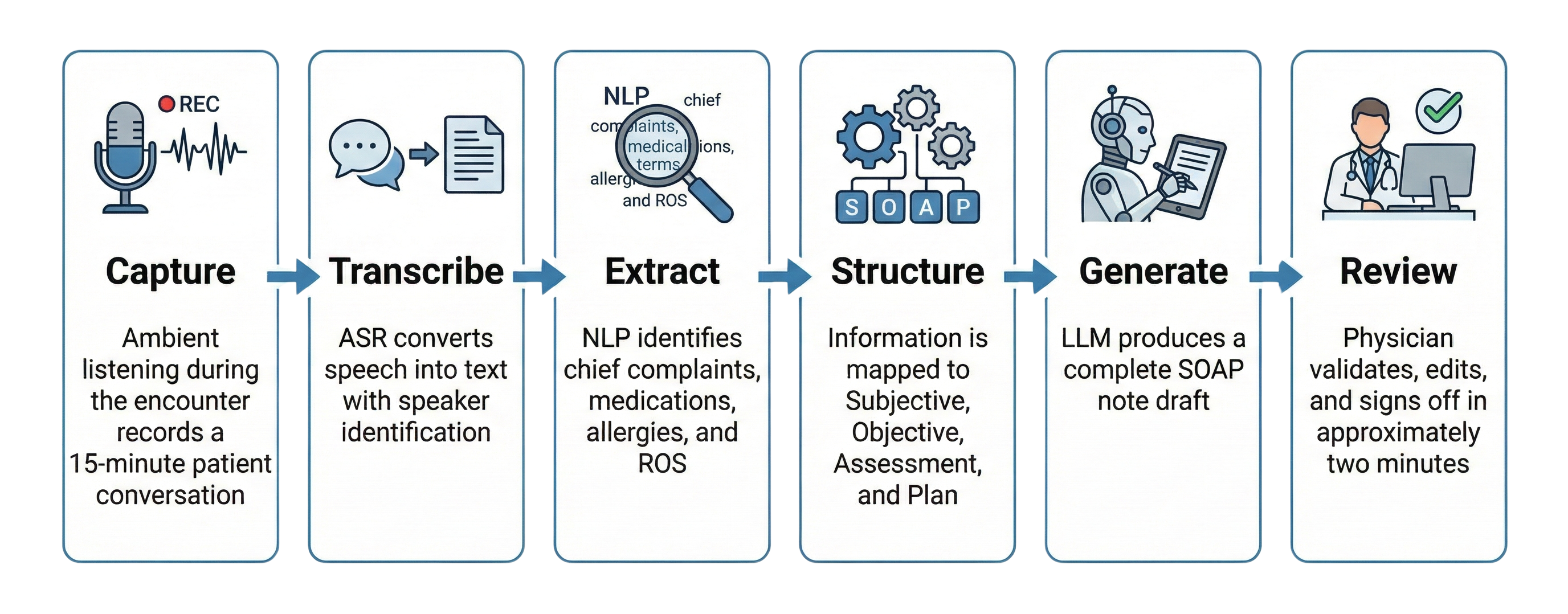
How AI Clinical Note Generation Works
Step-by-Step Process
Key Capabilities of AI Documentation Tools
Ambient Clinical Documentation
AI systems passively listen to natural patient-provider conversations without requiring clinicians to dictate or manually enter data.
Multi-Template Support
Automatically formats notes into SOAP, H&P, progress notes, or specialty-specific templates based on encounter type.
Clinical Decision Support
Provides diagnostic suggestions, flags potential drug interactions, and prompts clinicians to address missing documentation elements.
ICD-10 and CPT Code Suggestions
Analyzes documentation to recommend accurate billing codes, improving claims accuracy and revenue capture.
EHR Integration
Seamlessly integrates with leading EHR platforms such as Epic, Cerner, and Athena, pushing notes directly into the patient record.
Benefits of AI-Powered Clinical Documentation
| Benefit | Impact |
| Time Savings | Reduces documentation time by 50 to 75 percent |
| Improved Note Quality | Produces more complete and consistent documentation |
| Reduced Physician Burnout | Allows clinicians to focus on patients instead of keyboards |
| Better Patient Experience | Enables more eye contact and deeper engagement |
| Enhanced Compliance | Ensures required regulatory elements are captured |
| Revenue Optimization | Supports accurate coding and billing |
Challenges and Key Implementation Considerations
Critical Factors for Successful Adoption
- Accuracy Validation
AI-generated notes still require physician review and final attestation. - HIPAA Compliance
All audio and text data must be encrypted and managed in accordance with PHI regulations. - Bias Mitigation
Models must be trained on diverse patient populations to reduce bias. - Workflow Integration
Seamless EHR integration is essential for clinician adoption and efficiency. - Specialty Customization
Templates and models must adapt to different clinical workflows and specialties.
Are Clinical Notes Legal Documents?
Yes, clinical notes are legal documents and may be reviewed by third parties in a variety of legal, regulatory, and administrative situations. Because clinical notes form part of the official medical record, they carry significant legal and professional weight.
Clinical notes may be reviewed during:
- Insurance audits, to verify medical necessity and appropriate billing
- Regulatory investigations, including reviews by government or accrediting agencies
- Malpractice litigation, where documentation is used to evaluate the standard of care
- Licensing or credentialing reviews, to assess professional conduct and competence
Because of their legal significance, clinical notes must meet high standards of accuracy and professionalism.
Clinical notes should always be:
- Accurate and objective, clearly reflecting clinical findings without speculation or bias
- Timely and complete, documenting care as close to the time of service as possible
- Free from judgmental, emotional, or inappropriate language, which could be misinterpreted if reviewed
High-quality clinical documentation not only supports patient care but can also significantly reduce legal, financial, and compliance risks for healthcare professionals and organizations.
Common Clinical Documentation Mistakes (and How to Avoid Them)
Even experienced healthcare providers can make documentation errors, and these mistakes can affect patient care, compliance, and legal defensibility. Recognizing common pitfalls is the first step toward improving documentation quality.
Common clinical documentation mistakes include:
- Incomplete or vague notes, which can create gaps in patient care and raise questions during audits or reviews
- Overuse of copy-and-paste, increasing the risk of outdated, inaccurate, or contradictory information
- Missing signatures or timestamps, which may invalidate documentation for legal or billing purposes
- Subjective or emotional language, which can appear unprofessional or biased if notes are reviewed
- Delayed documentation, leading to reduced accuracy and increased compliance risk
How to prevent documentation errors:
Using standardized templates, documenting care promptly, and routinely reviewing notes for clarity and accuracy can significantly reduce these issues. Consistent documentation practices help ensure clinical notes remain accurate, defensible, and aligned with professional standards.
Frequently Asked Questions About Clinical Notes
Who can write a clinical note?
Clinical notes are written by licensed healthcare professionals who are directly involved in a patient’s care. This may include physicians, nurses, mental health providers, therapists, nurse practitioners, and physician assistants, depending on the care setting and scope of practice.
How long should clinical notes be retained?
Clinical note retention requirements vary by jurisdiction, organization, and care setting. In many cases, records must be retained for 7–10 years or longer, particularly for minors or in situations involving legal or regulatory requirements.
What’s the difference between a clinical note and a progress note?
A clinical note is a broad term that refers to any formal documentation within a patient’s medical record. A progress note is a specific type of clinical note that focuses on documenting a patient’s status, response to treatment, and changes in care over time.
Can patients access their clinical notes?
Yes. In many regions, patients have a legal right to access their medical records, including clinical notes. Patient access is often governed by healthcare privacy laws and regulations, such as those related to health information rights and transparency.
Conclusion: Why High-Quality Clinical Notes Matter
Clinical notes are far more than administrative records, they are essential tools that support patient safety, clinical decision-making, regulatory compliance, and effective communication across healthcare teams. Understanding what a clinical note is, and how to write one clearly and accurately, benefits patients, healthcare providers, and organizations alike by improving care quality and reducing risk.
Strengthen Your Clinical Documentation Practices
High-quality clinical notes are essential for patient safety, regulatory compliance, and effective care coordination. As documentation requirements continue to evolve, healthcare organizations must ensure their clinical note practices remain accurate, efficient, and aligned with current standards.
Now is the ideal time to review documentation workflows, evaluate note quality and consistency, and equip clinical teams with the tools and training needed to support clear, defensible clinical documentation—including emerging AI-powered solutions.
For expert support in improving clinical documentation practices and optimizing clinical note workflows, specialized guidance is available.
📞 Phone: +1 (727) 214-2749
📧 Email: success@medviz.ai
Leave a Reply