Why EDI is More Essential Than Ever in Medical Billing
In 2025, healthcare providers are under increasing pressure to cut costs, improve claim accuracy, and meet strict compliance requirements. Manual billing processes are slow, error-prone, and costly. That’s where Electronic Data Interchange (EDI) steps in—offering an efficient, secure, and standardized way to manage medical claims and insurance transactions.
This guide breaks down everything you need to know about EDI in medical billing, including how it works, its key benefits, major transaction types, implementation tips, real-world examples, and future trends shaping the industry.
What is EDI in Medical Billing? A Modern Definition
Electronic Data Interchange (EDI) is the digital exchange of standardized healthcare data between medical providers, payers (insurance companies), and clearinghouses. Instead of relying on paper or fax, EDI automates the communication process using structured file formats like ANSI X12, ensuring fast and accurate data transmission.
In the medical billing space, EDI supports functions such as:
- Submitting insurance claims
- Receiving payment remittances
- Verifying patient eligibility
- Requesting authorizations
- Tracking claim statuses
EDI is not only efficient—it’s HIPAA-compliant, making it a mandatory element in most modern healthcare billing systems.
Why EDI Matters: Key Benefits for Healthcare Providers
Healthcare organizations using EDI benefit from significant improvements in cost, speed, and compliance. Here’s how EDI transforms medical billing:
💰 Reduced Administrative Costs
- Providers save an average of $1.49 per claim, and hospitals save $0.86 by switching from paper to electronic claims (CAQH Index).
- Over time, these savings scale dramatically for high-volume practices.
⏱ Faster Claims Processing
- Electronic claims are often processed in real time or within 24 hours, compared to several days or weeks for manual submissions.
✔️ Fewer Errors and Rejections
- EDI uses standardized formats that reduce claim rejections caused by:
- Incomplete data
- Formatting issues
- Incorrect coding
🔒 Improved Data Security and Compliance
- EDI transactions are encrypted and aligned with HIPAA standards, reducing the risk of data breaches and legal issues.
Key EDI Transactions in Medical Billing
Understanding common EDI transaction codes is crucial for managing the medical billing lifecycle. Here’s a quick guide:
| Transaction Code | Function |
| 837 | Insurance claims submission |
| 835 | Payment and remittance advice |
| 270/271 | Eligibility request and response |
| 276/277 | Claim status inquiry and response |
| 278 | Authorization and referral requests |
| 834 | Enrollment and benefits administration |
These codes are used across all payers and clearinghouses, forming the foundation of digital healthcare communication.
How EDI Works in the Medical Billing Workflow
EDI is embedded throughout the medical revenue cycle, from patient check-in to final payment reconciliation:
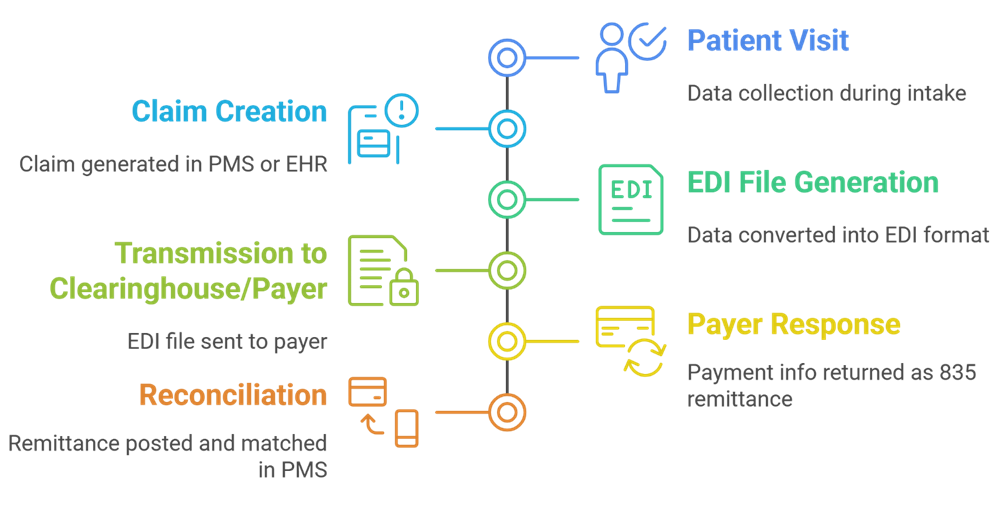
By eliminating manual entry and mail-based processing, EDI reduces turnaround time and improves claim acceptance rates.
How to Implement EDI in Your Practice: 2025 Best Practices
If you’re considering EDI for your medical practice or organization, follow these steps for a smooth transition:
✅ Assess Your Current Technology
- Does your EHR or PMS support EDI transactions?
- Can it export and read ANSI X12 file formats?
✅ Select a Trusted EDI Clearinghouse or Vendor
- Look for HIPAA-compliant, cloud-based platforms with:
- Real-time tracking
- Built-in claim scrubbing
- Strong customer support
✅ Train Billing Staff
- Ensure your team understands:
- EDI transaction codes
- Rejection management workflows
- Proper data entry for clean claims
✅ Monitor Key Performance Metrics
- Focus on:
- Clean claims rate
- Days in A/R
- Denial rates and resolution time
✅ Test Before Going Live
- Run sample claims to detect mapping errors and ensure smooth integration
Common EDI Challenges (and How to Overcome Them)
Despite its advantages, EDI isn’t without hurdles. Here’s how to navigate them:
❗ Data Mapping Issues
- Incompatible fields can cause rejections.
- Solution: Use middleware or custom mapping tools.
❗ Integration with Legacy Systems
- Older PMS may not support modern EDI standards.
- Solution: Consider cloud-based or API-enabled platforms.
❗ Staff Resistance
- New workflows can be intimidating.
- Solution: Offer thorough onboarding, training, and role-based SOPs.
EDI Trends to Watch in 2025 and Beyond
The healthcare industry continues to evolve—and so does EDI. Key innovations include:
🌐 Cloud-Based EDI
- Scalable, cost-effective, and easier to maintain than legacy systems.
🔗 API + FHIR Integration
- APIs are beginning to complement traditional EDI, enabling real-time data exchange with FHIR protocols.
🤖 AI-Powered Automation
- Artificial intelligence helps:
- Predict denials
- Automate coding
- Optimize revenue cycle management
While APIs and AI are promising, EDI remains essential for payer communication and HIPAA compliance.
Conclusion: Is Your Practice Ready for EDI in 2025?
EDI is the digital backbone of modern medical billing. Whether you’re a small clinic or a large hospital, integrating EDI can:
- Speed up claims
- Reduce errors
- Lower operational costs
- Ensure regulatory compliance
Now is the time to evaluate your billing system and explore an EDI-enabled solution that supports your goals in 2025 and beyond.
Get Ready for the Future of Medical Billing with Medviz.ai
As healthcare in 2026 evolves—with rising costs, complex payer policies, and growing patient expectations—now is the time to future-proof your practice. Medviz.ai combines AI-powered billing, expert RCM support, and a patient-first mindset to help providers maximize reimbursements, reduce denials, and improve satisfaction across the board.
Whether you’re looking to streamline EDI processes or gain deeper insights into your revenue cycle, Medviz.ai is your partner in progress.
👉 Call us today at +1 (727) 214-2749
📩 Or email us at success@medviz.ai
Power your practice’s success with Medviz.ai—where innovation meets results.
Leave a Reply